The Journal of Medical Ethics recently published research by Clive Searle: "The role of doctors’ religious faith and ethnicity in taking ethically controversial decisions during end-of-life care." The full paper is only available to subscribers. (A doctor kindly forwarded me a copy to read but obviously I can't put it on the internet myself.) There is an abstract freely available online.It is high time that the moral implications of atheism be examined and the effect of atheism on the behavior of professionals in our society be taken into account and not assumed to be "normal" or "neutral." Atheism is, in fact, a social scourge.
One of the findings of the research summarised in the abstract is that:Independently of speciality, doctors who described themselves as non-religious were more likely than others to report having given continuous deep sedation until death, having taken decisions they expected or partly intended to end life, and to have discussed these decisions with patients judged to have the capacity to participate in discussions.The reporting of this research has been subject to spin that Private Baldrick might describe as "like a very spinning thing." So the BBC reports: Religion may influence doctors' end-of-life care. The report offers the following reassurance:While it is illegal to give drugs with the deliberate intention of ending someone's life, doctors may administer morphine or other medication to relieve pain or distress which may have the effect of shortening life - so-called deep sedation.This rather ignores the finding of the research that non-religious doctors were in fact taking decisions that they "partly intended" to end life. Certainly this is supposed to be illegal according to the Mental Capacity Act. But we knew all along that the MCA would lead to doctors taking decisions that were intended to end life. This has been happening for quite some years now and the MCA has made it easier to get away with it.
The obvious conclusion that the MCA has in fact led to euthanasia by the back door is ignored in favour of subtly attacking doctors who do have a religious faith, implying that they do not take into account the patient's needs or best interests. In Britain today, it is accepted that a patient's "best interests" might be to die, whereas a doctor who believes in the sanctity of life, the hippocratic oath or other such unfashionable concepts might well consider that intending to end a patient's life is a perversion of any reasonable understanding of their "best interests." The spin given to the reporting of Clive Searle's research is a clear hint that "religious" doctors should be controlled and prevented from having so much influence in the palliative care of the dying.
At the Outside In blog by Catholic father, Michael Merrick, there is a good article analysing the BBC report: BBC: bringing Dignity to a death near you. Anglican Bishop Nick Baines also writes: Shock report: faith affects choices! fisking the BBC report. He makes the important point:Conscious atheism or agnosticism should demonstrate equal consistency and be examined for inherent weakness in the same way as religious beliefs should be subjected to rigorous scrutiny. But, atheism cannot simply be assumed to be the neutral default position from which any other ‘belief’ is a dangerous deviation.In fact, the full text of the research paper (not available on the internet without subscription) actually acknowledges this:One potential response to the findings about the influence of religious faith is to suggest, as other have done, that religious doctors disclose their moral objections to certain procedures to patients so that patients can choose other doctors if they wish. This assumes that religiosity is the ‘exception’ to be set against the non-religious ‘norm’. It is equally plausible to argue that non-religious doctors should confess their predilections to their patients.Despite this important qualification in the paper itself, the British Medical Association said:The religious beliefs of doctors should not be allowed to influence objective, patient-centred decision-making. End-of-life decisions must always be made in the best interests of patients.Following Bishop Baines, we should require that the BMA recognise that the atheist beliefs of doctors should not be allowed to influence objective, patient-centred decision-making. Particularly when they are nearly twice as likely to kill you intentionally on request as the research finds.
Sunday, August 29, 2010
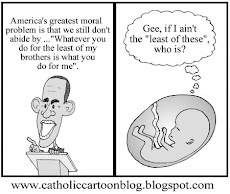
Study Says That Atheist Doctors are More Likely to Kill You
Fr. Tim Finigan at the blog, The Hermeneutic of Continuity, has a very interesting article on a recent study published in the Journal of Medical Ethics on the issue of how atheist doctors are more likely to commit euthanasia than non-atheists. It deserves to be quoted extensively and makes for fascinating reading.
Subscribe to:
Post Comments (Atom)




No comments:
Post a Comment